[NS21] Mental Illness
cf. 옛날에 구분:
- Neurology(신경과): concerned with the diagnosis and treatment of nervous system disorders
- psychiatry(정신과): Concerned with the diagnosis and treatment of disorders affecting the mind (psyche)
we discuss some of the most severe and prevalent psychiatric disorders: anxiety disorders, affective disorders, and schizophrenia.
We will see that a great deal can be learned about the nervous system by studying what happens when things go wrong.
(print-introduction 생략…)
3? categoeries of psychiatric disorders:
- Mental Illness
- Anxiety disorders
- Mood disorders
- Schizophrenia
- Prevalence: The proportion of a population wth a condition
- Lifetime prevalence: The proportion of a population that will experience the condition at some point during their lives.
- comorbidity: 같이 수반되는 것.
1. Mental Illness & the Brain
Mental Illness(disorder)
1.1. Psychosocial Approaches to Mental Illness
Behaviorism: Ignore the notions of underlying conflicts and the unconsciousness and focus on the observable behaviors.
e.g. B. F. Skinner
1.2. Biological Approaches to Mental Illness
general paresis of the insane
Initially blamed on psychological factors, the cause was eventually traced to infection of the brain with Treponema pallidum, the microorgamism that causes syphilis.
penicillin: selectively killing the pathogen => Major psychiatric disorder virtually eliminated.
(etc. about molecular medicine in psychiatry.)
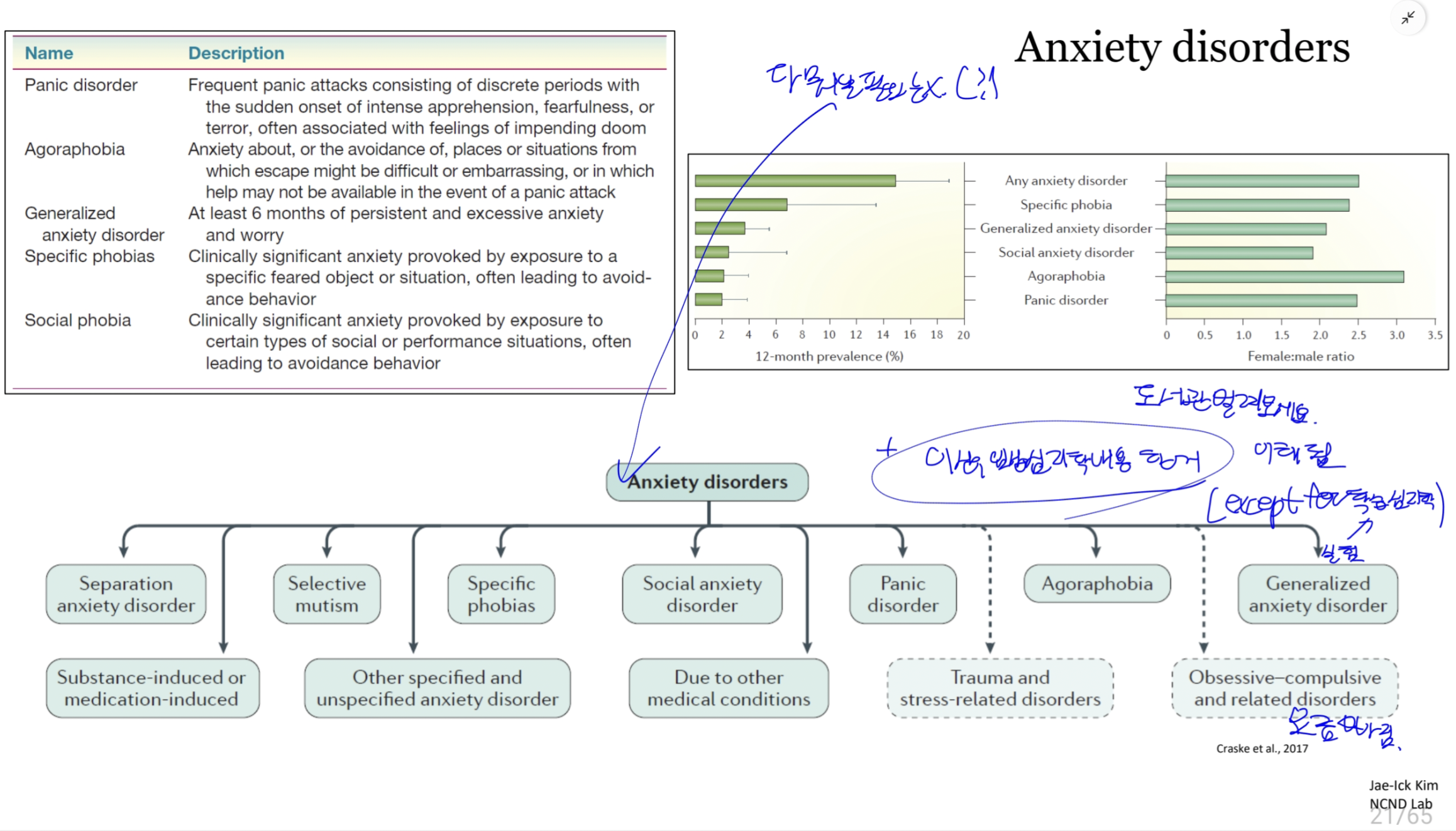
2. Anxiety Disorders
Definition: Inappropriate expression of fear.
Most common psychiatric disorders.
cf. key epidemiology of anxiety disorders 1) Prevalence: 1 in 4 individuals are likely to have or have had anxiety disorders. 2) Age at onset: mostly starting early in life (especially phobias and separation anxiety) -> some anxiety disorders can emerge late in life (generalized anxiety disorder) 3) Culture-specific anxiety disorders (Taijin kyofusho, Japanese) 4) Vulnerability and risk factors: female sex, a family history of anxiety, depressive disorders
Categories
2.1. A description of Anxiety Disorders
The pathological expression of fear.
2.1.1. Panic Disorder
Panic attacks: sudden feelings of intense terror occuring without warning.
- Symptoms: palpitations, sweating, trembling, shortness of breadth, chest pain, nausea, dizziness, tingling sensations, chills, blushing
- Characterized by recurring, seemingly unprovoked panic attacks and a persistent worry about having future attacks.
- Reporting an overwhelming fear that they are dying or “going crazy”
Panic disorder: recurring, seemingly unprovoked panic attacks and a persistent worry about having further attacks.
cf. Epidemiology
- 2% of the population
- Common in women (twice)
- Onset: most common after adolescence (but before the age of 50)
- 50% of patients having panic disorders will also suffer from major depression.
2.1.2. Agoraphobia
characteristic: Severe anxiety about being in situations where escape might be difficult or embarassing. Causing avoidance of places or situations that might cause you to panic.
Symptoms: fearing an actual or anticipated situations, such as using public transportation, being in open or enclosed spaces, standing in line, being in a crowd
Epidemiology
- 5% of the population
- Common in women (twice)
-
Onset: usually starting in early adult years
- Risk factors: 1) Having panic disorder or other phobias 2) Experiencing stressful life events 3) Having an anxious or nervous temperament 4) Having a blood relative with agoraphobia
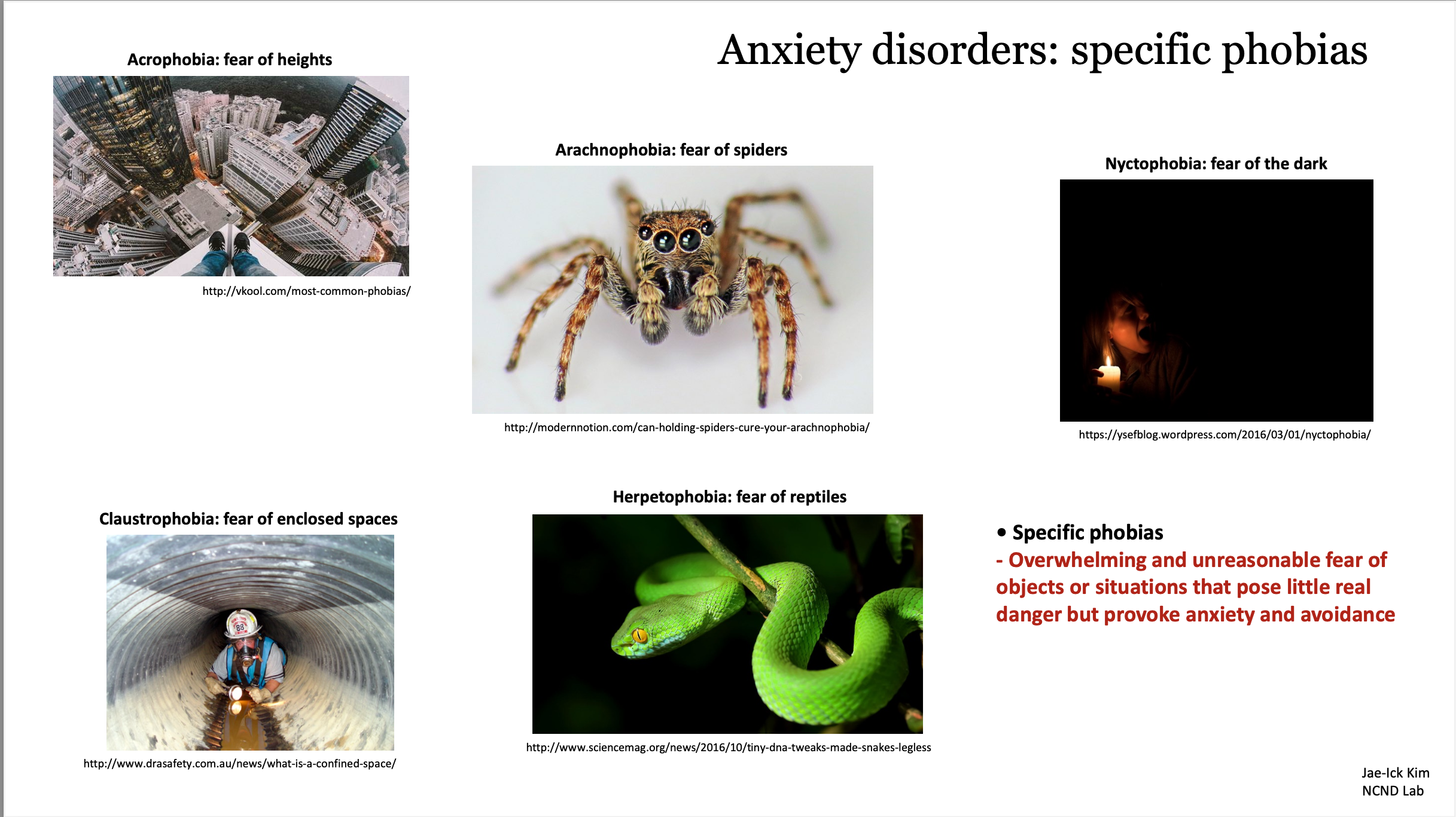
2.1.3. Specific Phobias
Specific Phobia:
Overwhelming and unreasonable fear of objects or situations that pose little real danger but provoke anxiety and avoidance
Examples:
- Acrophobia: fear of heights
- Arachnophobia: fear of spiders
- Nyctophobia: fear of the dark
- Claustrophobia: fear of enclosed spaces
- Herpetophobia: fear of reptiles
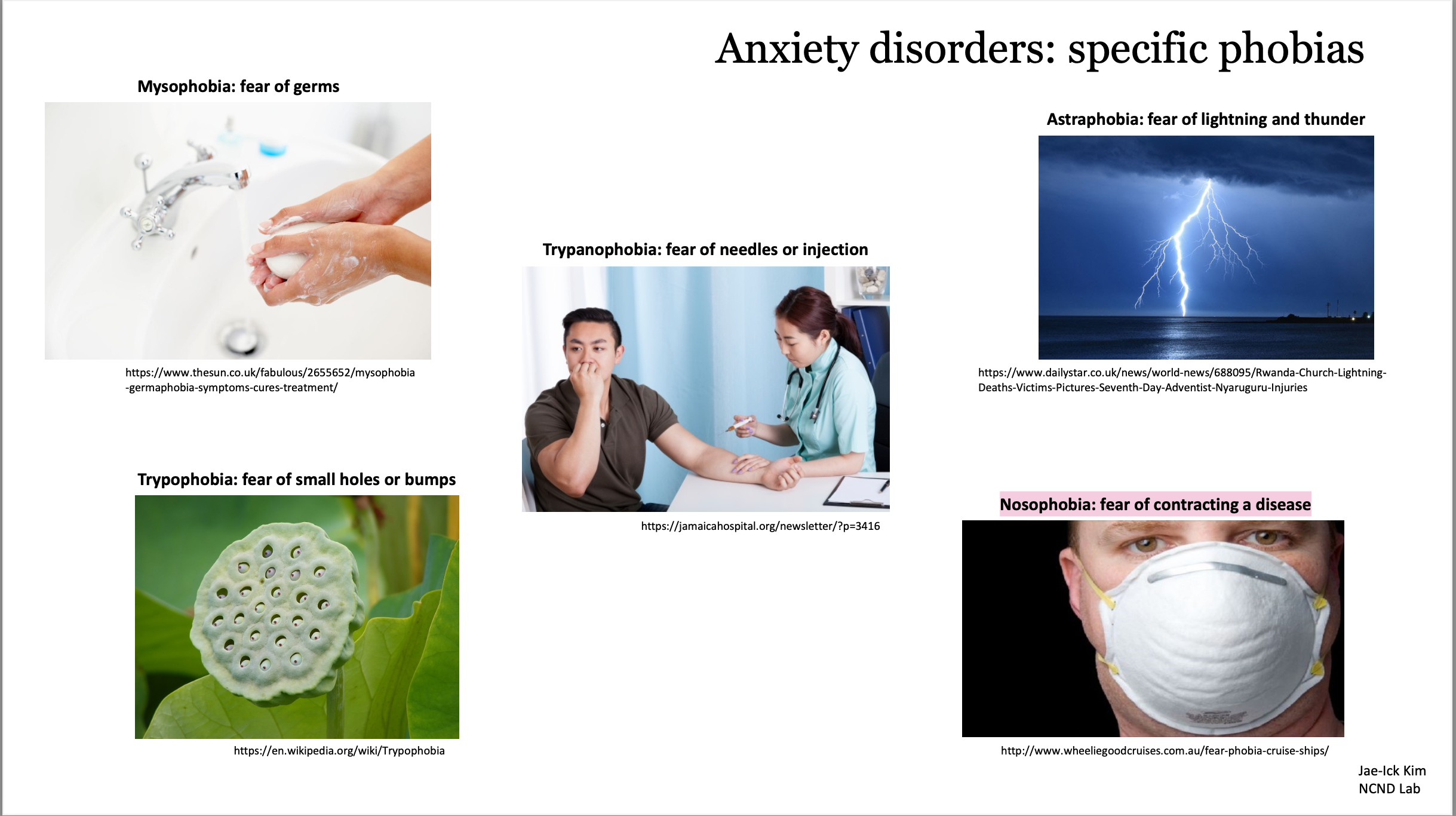
- Mysophobia: fear of germs
- Trypophobia: fear of small holes or bumps
- Trypanophobia: fear of needles or injection
- Astraphobia: fear of lightning and thunder
- Nosophobia: fear of contracting a disease
2.1.4. social phobia
Social anxiety disorder (social phobia)
- Characterized by a significant amount of fear or anxiety in one or more social situations
- Symptoms: considerable distress and impaired ability to function in at least some parts of daily life
2.2. Other disorders Characterized by Increased Anxiety
2.3. Biological Bases ofAnxiety Disorders
2.4. Treatments for Anxiety Disorders
3. Affective Disorders (mood disorders)
Affect; medical term for emotional state or mood.
Affective Disorders: disorders of mood. (mood disorders)
Changes in mood are more long-lasting and much more severe (than the ones in normal people).
- Major depressive disorder, bipolar disorder, persistent depressive disorder (dysthymia), seasonal affective disorder (SAD), depression induced by substance use
cf. Key epidemiology of affective disorders 1) Prevalence: 9% of population 2) Age at onset: mid-teens to late 20s 3) Vulnerability and risk factors: family history (genetics), stressful event or major life change (environment)
(pp.37/65)
3.1. A Description of Affective Disorders
3.1.1. Major Depression
Major symptoms: A persistent feeling of sadness, lower mood, decreased interest or pleasure in all activities (must be present every day for at least 2 weeks)
Other symptoms:
- loss of appitite
- insomnia
- fatigue
- feelings of worthless and guilt
- diminished ability to concentrate
- recurrent thoughts of death
(Main precipitating cause of suicide)
This is not a sign of weakness (we cannot simply snap out of it.) e.g. 떡볶이 먹고 기분 풀 생각이 안된다.
Requiring long-term treatment, X last longer than 2 years. Recurring in 50% of cases without treatment.
Possible causes: biological differences in the brain, neurotransmitters, hormones, inherited genes.
cf. Epidemiology
- 6% of population
- Common in women (twice)
- Onset: usually beginning in the tees, 20s, or 30s (but can happen at any age)
- Risk factors: 1) Family history 2) Stressful life events
dysthymia: milder, chronic ones.
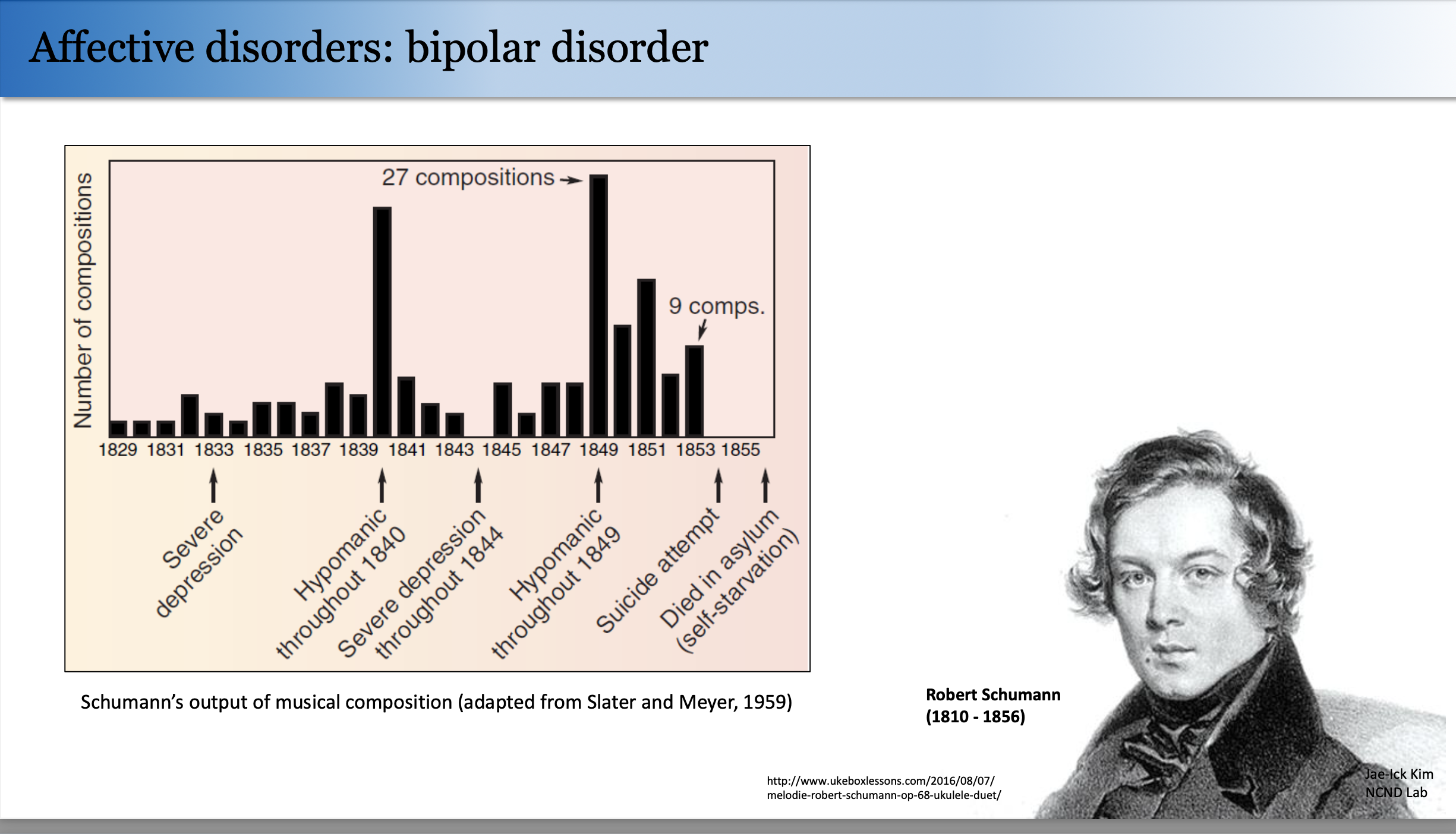
3.1.2. Bipolar Disorder
Characterized by repeated episode of mania, or mixed episodes of mania and depression. (manic depressive disorder)
Mania: distinct period of abnormally and persistently elevated, expansive, or irritable mood
symptoms during the manic phase: inflated self-esteem, a decreased need for sleep, increased talkativeness, flight of ideas, distractibility, increased goal-directed activity.
Type I bipolar disorder
- Characterized by the manic episodes (with or without major depression)
- 1% of the population
- Equally in women and men
Type II bipolar disorder
- Characterized by hypomania (milder form of mania that is not associated with marked impairments in judgment or performance)
- 0.6% of the population
- Sometimes showing a marked increase in efficiency, accomplishment, or creativity
- Always associated with episodes of major depression
cf. even milder no ‘major’ (i.e. fewer symnptoms and shorter duration) depression => cyclothymia.
3.2. Biological Bases of Affective Disorders
3.2.1. The Monoamine Hypothesis
: The idea that the Monoamine transmitters (5-HT, NE) plays an important role in moods, and the defict in one of its DMS causes Depression. (참고로 기분은 DA보다는 5-HT나 NE에 영향을 더 크게 받는다.)
- Evidences
• Evidence 1: reserpine (VMAT inhibitor)
- Used as a vasodilator
- Depleting catecholamines and serotonin
- Causing severe depression (~20% of cases)
• Evidence 2: MAO inhibitors
- Inhibiting MAO that destroys catecholamines and serotonin
- Causing a marked mood elevation
• Evidence 3: imipramine
- Inhibiting the reuptake of released serotonin and norepinephrine -> promoting their action at synapses
- Used as an antidepressant
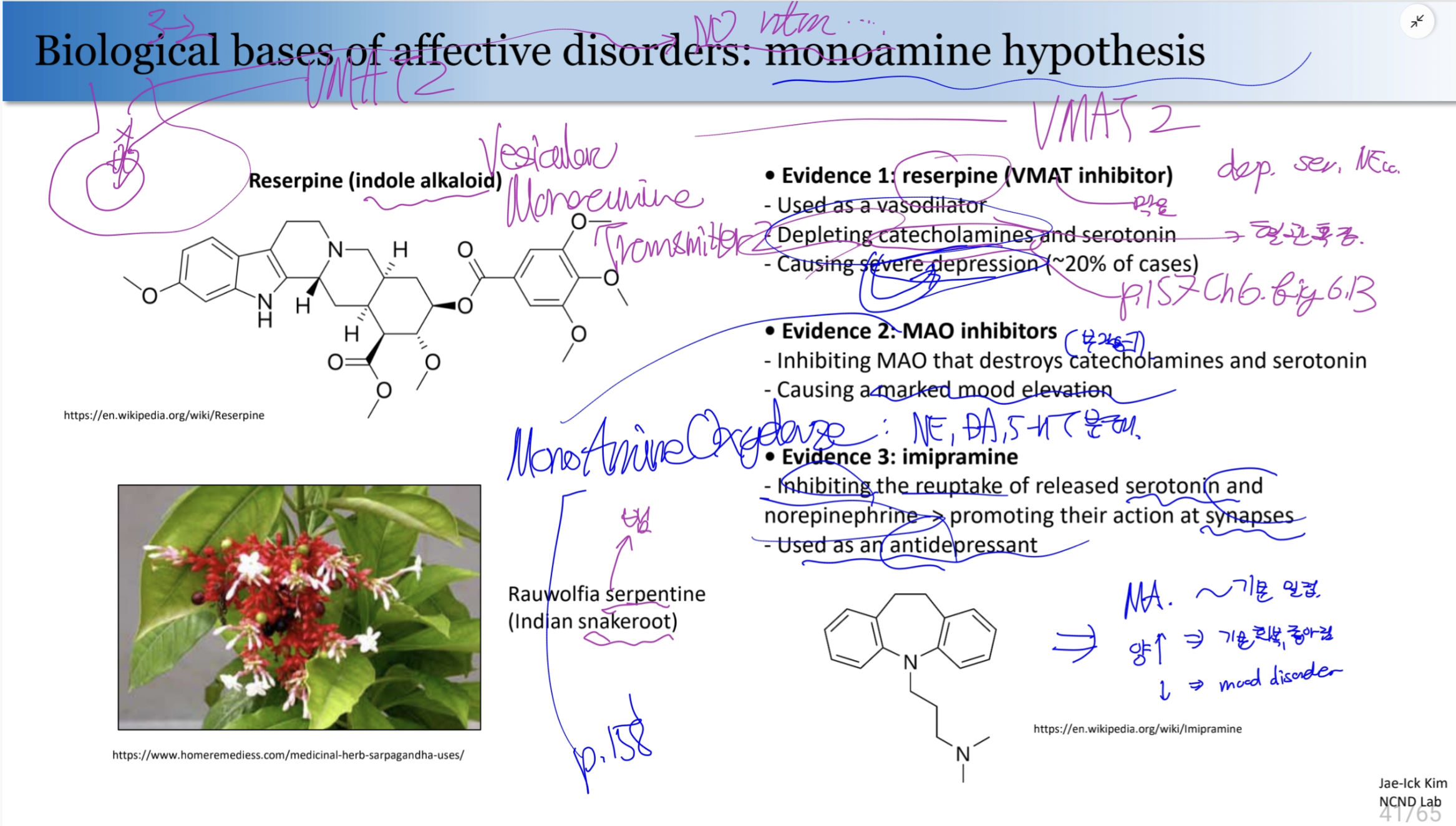
- Criticism
- Too simplistic
Antidepressant action of the drugs elevating 5-HT or NE takes several weeks to develop, even if they have almost immediate effects on transmission at the modulatory synapses.
(Hence, they may promote long-term adaptive changes in the brain.)
- Other drugs that raise NE levels in the synaptic cleft, like cocane, are not effective as antidepressants.
3.2.2. The Diathesis-Stress Hypothesis
diathesis: (타고나는) 소양, 기질
HPA axis is the main site of convergence between genetic and environmental factors causing mood disorders.
High comorbidity(coexisting rate?) between anxiety and depression.
Severely depressed patients: Exhibit hyperactivity of HPA axis. (with elevated blood cortisol levels, CRH concentrations in the CSF.)
• Evidences 1) Injection CRH into the brains of animals causing behavioral phenotypes similar to those of depression and anxiety. 2) The regulation of HPA axis by hippocampus is disrupted in depressed patients. -> Showing decreased number of glucocorticoid receptors (in hippocampus) -> The number of glucocorticoid receptors are regulated by genes, monoamines, and early childhood experience (early maternal care and tactile stimulation during critical period).
- Early childhood abuse and neglect, together with genetic factors -> putting people at risk for developing mood and anxiety disorders
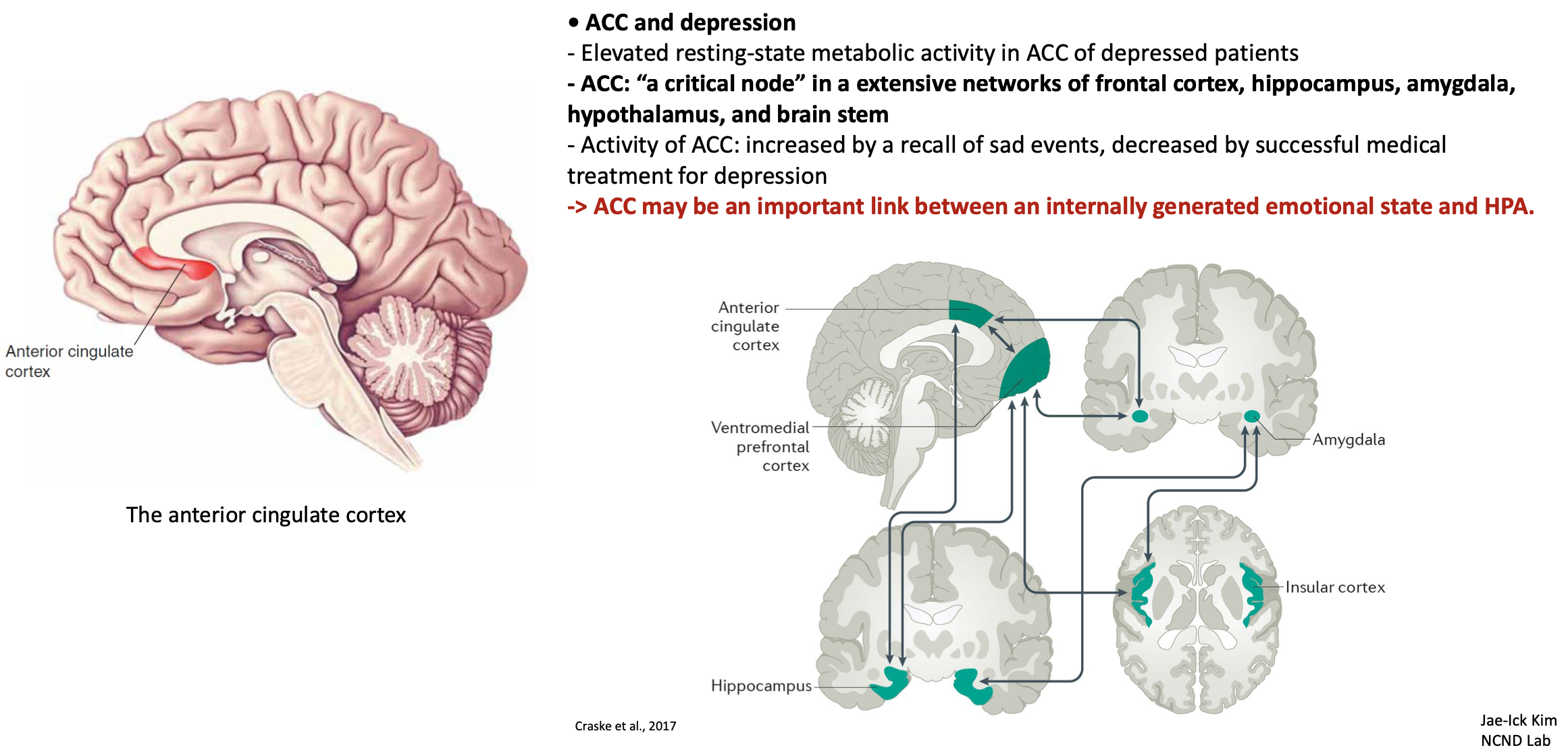
3.2.3. ACC(Anterior Cingulate Cortex) dysfunction
Depressed patients fMRI showed increased resting-state metabolic activity in ACC.
ACC: A critical node in an extensive network of frontal cortex, hippocampus, amygdala, hypothalamus, and brain stem.
hypothesis: ACC dysfunction contributes to the symptoms of major depression
evidences
Activity of ACC
- Increased by a recall of sad events.
- Decreased by a successful medical treatment for depression
3.3. Treatments for Affective Disorders
3.3.1. Electroconvulsive Therapy
- Initially introduced (1903s) by the mistaken belief that epilepsy and schizophrenia could not coexist in the same person
- Triggering seizure discharges by local electrical stimulation (temporal lobes)
- Performed especially when suicide risk is high
- Advantage: quick relief
- Disadvantage: temporary memory loss (past (6 months) and future), cognitive impairment
- Mechanism of action: unknown
3.3.2. Psycotherapy
- Effective in treating mild-moderate cases of depression.
- Help depressed patients overcome negative views of themselves and their future.
- Unknown neurobiological basis.
3.3.3. Antidepressants
3.3.4. Lithium
3.3.5. Deep Brain Stimulation
4. Schizophrenia
cf. Key epidemiology of anxiety disorders 1) Prevalence: 1% of population 2) Age at onset: during adolescence or early adulthood(earlier in males) 3) Sex: 1.4 times more common in males than females 4) Vulnerability and risk factors: family history (genetics), living environment, substance use, developmental factors
4.1. A Description of Schizophrenia
A loss of contact with reality, severely distorted thoughts, perceptions, mood, and movement.
Major public health problem. Many variations in the manifestations of the disorder.
2 symptoms:
- Positive symptoms (이왜있)
- Delusions (망상) e.g. 피해망상, 과대망상
- Hallucinations (a subset of delusion) 감각인지 잘못됨.
- Disorganized Speech
- Grossly disorganized or catatonic behavior (횡설수설/축처짐)
- Negative Symptoms (이왜없) (observation is hard… 치료 hard.)
- Reduced expression of emotion
- Poverty of speech (말수 적음. like 치매)
- Difficulty in initiating goal-directed behavior (~해야하니 ~하기)
- Memory impairment (상실)
4.2. Biological Bases of Schizophrenia
4.2.1. Genes and the Environment
(프린트-p.58/65)
Genetic factors in schizophrenia
- Schizophrenia runs in families.
- Most of genes predisposing people to schizophrenia play important roles in synaptic transmission, plasticity, and the growth of synapses.
Environmental factors in schizophrenia 1) Maternal stress during pregnancy -> Infections and immune challenge, poor nutrition, hypoxia(저산소증) 2) Environmental stress -> Substance use, social isolation (집가도 아무도 없을 때), family dysfunction, unemployment (실직)

.png)